-
 Laboratory for molecular and translational nephrology
Laboratory for molecular and translational nephrologyTobias B. Huber
Mission Statement
“Enabling and performing excellence in clinical and molecular nephrology”
— Tobias B. Huber, MD
Team Members
Marigona Agushi
Karl King Alornyo

Fabian Braun, MD
Berk Cantutan
Silvia Chilla

Jan Czogalla, MD
Ilka Edenhofer

Tilo Freiwald, MD
Sydney Gies, MD

Maja Gunkel
Yubing Guo
Sonja Hänzelmann, PhD
Paris Hazelton-Cavill
Felicitas Hengel, MD
Julius Jäger

Sybille Köhler, PhD

Inga Komisarenko

Oliver Kretz, MD

Sandra Laufer, PhD
Dinh To Le, PhD

Samaneh Liagos
Zhouning Liao
Nastassia Liaukouskaya
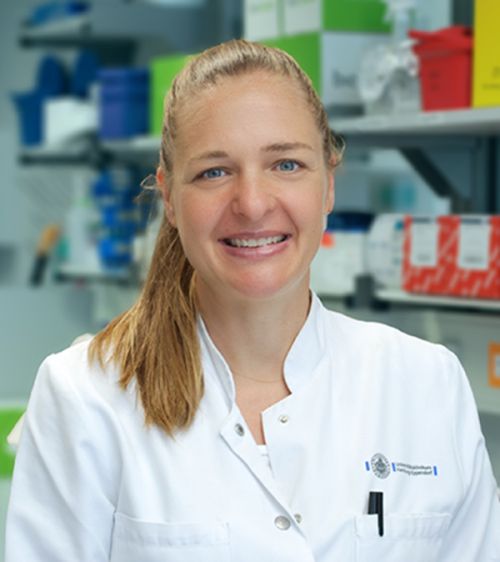
Maja Lindenmeyer, PhD
Shuya Liu, PhD
Shun Lu, PhD
Elisabeth Meister, MD

Ming Huang, PhD
Anne Mühlig, MD/PhD

Christiane Neuber, PhD
Y-lan Nguyen-Khanh
Valerie Oberüber

Anja Obser

Alexander Pausch

Melanie Schaper

Christian Schmidt-Lauber, MD

Kristina Schulz, PhD
Nicola Wanner, PhD
Guochao Wu
Gunther Zahner, PhD
Nina Ziegert

Marina Zimmermann, PhD
Nikolay Zolotarev, PhD
Research
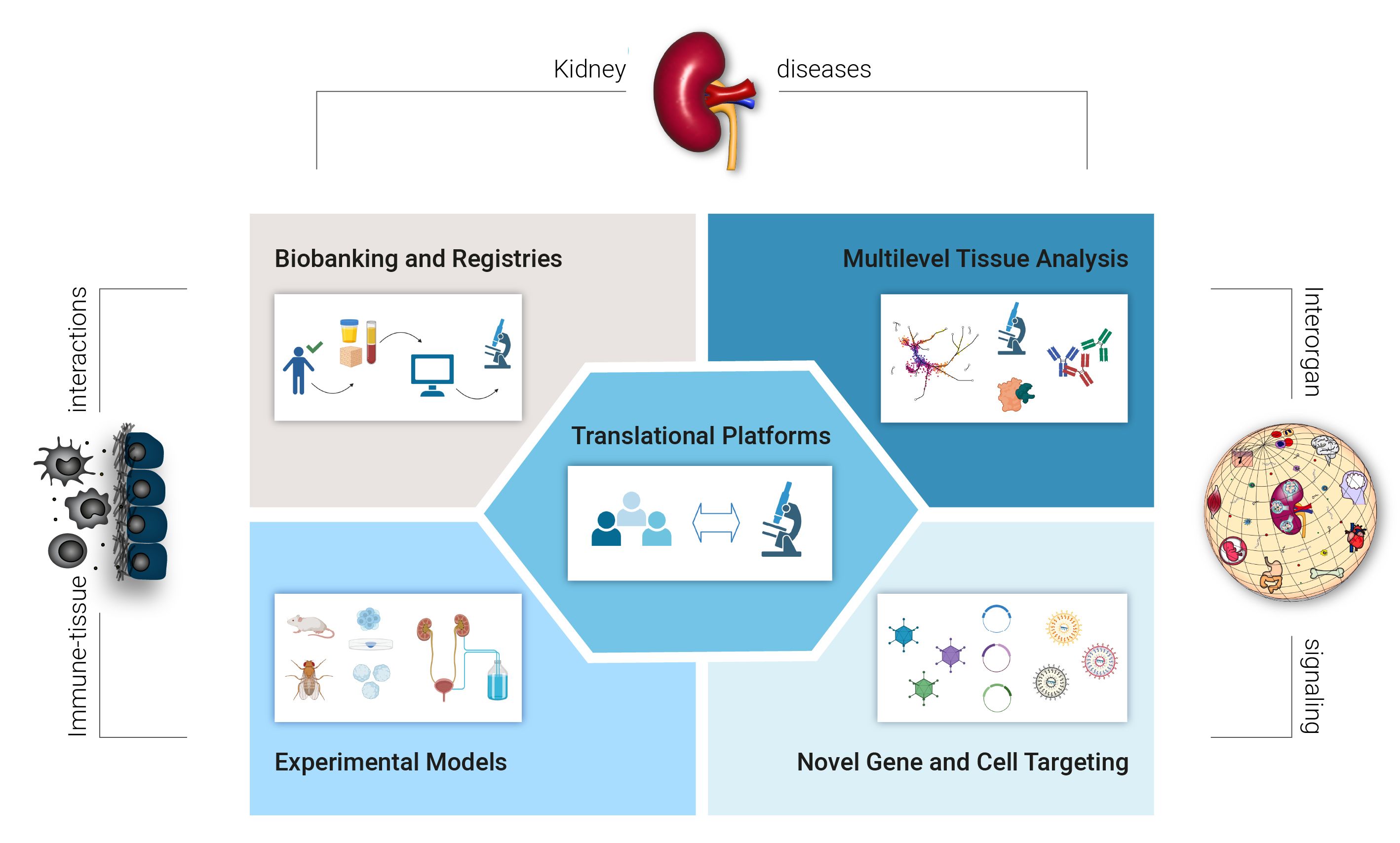
Created with BioRender
We aim at a better understanding of podocytopathies, the identification of complex principles of kidney diseases, immune -tissue interactions and interorgan signaling. For this purpose, our lab is advancing the following research areas:
- Modern tissue banks and patient registries by means of complex data analysis and attention to data security
- Multidimensional techniques for tissue analysis and single-cell biology
- Application and development of experimental models for the precise analysis of disease mechanisms
- New strategies of gene- and cell targeting in the kidney
- Development of translational platforms for the transfer of molecular findings into novel therapies
With this, our aim is to identify new approaches for the prevention, halt and cure of kidney diseases.
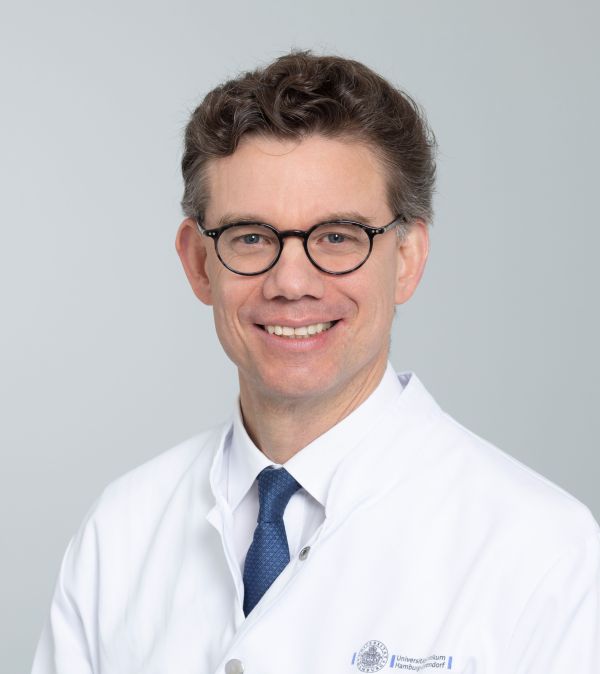
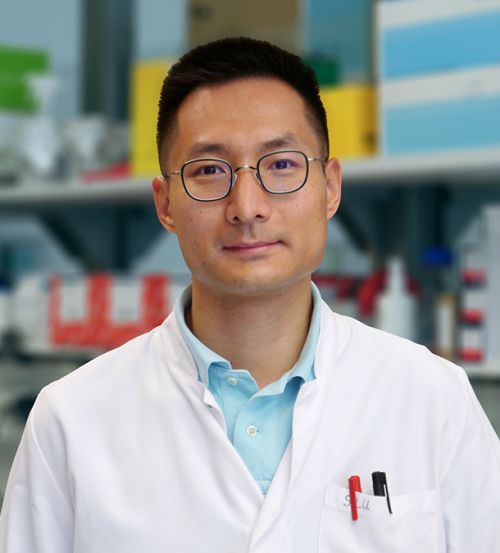
Tobias B. Huber, MD
Chair of the Center of Internal Medicine
Director of the III. Department of Medicine
III. Department of Medicine, University Medical Center Hamburg-Eppendorf (UKE)
Martinistr. 52
20246 Hamburg, Germany
CV
Chair of the Center of Internal Medicine
Director of the III. Department of Medicine
1992 - 1999 | School of Medicine (10/1992-05/1999), Universities of Freiburg, Vienna (Austria) and South Florida (Tampa, USA) |
2020 - 2020 | Chair of the Center of Internal Medicine, UKE |
2017 | Chair of the III. Department of Medicine, UKE |
2015 | Chief of the Division of Chronic Kidney Disease, University Medical Center Freiburg (UKF), Germany |
2013 | W3 Heisenberg Professor, UKF |
2008 | German Board Certification for Internal Medicine (2008) and Nephrology (2011) |
2007 | Habilitation, UKF |
2005 | USMLE US-American Full Medical Licence |
1999 | M.D. in Physiology (summa cum laude), Department of Physiology, UKF |
Clinical postgraduate education:
2015 - 2017 | Deputy Chair, Department of Medicine IV, UKF |
2011 - 2015 | Senior Attending (Geschäftsführender Oberarzt), UKF |
2008 - 2011 | Attending Physician, Department of Medicine IV, UKF |
2001 - 2003 | Fellow in Medicine, Department of Medicine IV, UKF |
1999 - 2001 | Residency, Department of Medicine IV, UKF |
Scientific postgraduate education:
2013 - 2017 | W3 Heisenberg Professorship, UKF |
2006 - 2011 | Emmy Noether Programme – Phase II / Group leader, UKF |
2003 - 2006 | Emmy Noether Programme – Phase I / Postdoctoral Fellow, Immunology & Pathology, Washington University St. Louis, USA (Laboratory of Prof. Dr. A. Shaw) |
2021 - 2020 | Elected Member of the National Academy of Sciences – Leopoldina- |
2021 | Elected Member of the American Association of Physicians |
2021 | Chair Else Kröner-Fresenius Clinician-Scientist Kolleg “iPRIME-CS”, UKE |
2021 | Co-Chair BMBF-Advanced Clinician Scientist Program “iSTAR”, UKE |
2020 | Speaker (together with U. Panzer) of the CRC 1192 |
2020 | DFG-Senate Commission on Key Questions in Clinical Research |
2018 | Chair Else Kröner-Fresenius MD-Thesis Kolleg “iPRIME”, UKE |
2016 | Co-Chair Else Kröner-Fresenius Kolleg “NAKSYS”, UKF |
2014 | Recipient of the European Research Council Grant |
2014 | Elected Member of the American Society of Clinical Investigation |
2012 | Young Investigator Award of the American Society of Nephrology (Considered the worldwide highest award for renal research < 45 years) |
2010 | Franz-Volhard Award of the German Renal Society |
2009 | Hans U. Zollinger Research Award of German Renal Society |
2008 | Associated Member of the BIOSS Excellence Cluster, Freiburg |
2006 | Principal Investigator of the SGBM Graduate School, Freiburg |
2004 | Carl Ludwig Award of the German Renal Society |
Selected publications
1. | Molecular consequences of SARS-CoV-2 liver tropism. |
2. | Pro-cachectic factors link experimental and human chronic kidney disease to skeletal muscle wasting programs. |
3. | Podocytes maintain high basal levels of autophagy independent of mtor signaling. |
4. | Decoding myofibroblast origins in human kidney fibrosis. |
5. | SARS-CoV-2 renal tropism associates with acute kidney injury. |
6. | Multiorgan and Renal Tropism of SARS-CoV-2. |
7. | Anaerobic Glycolysis Maintains the Glomerular Filtration Barrier Independent of Mitochondrial Metabolism and Dynamics. |
8. | ARP3 Controls the Podocyte Architecture at the Kidney Filtration Barrier. |
9. | The FERM protein EPB41L5 regulates actomyosin contractility and focal adhesion formation to maintain the kidney filtration barrier. |
10. | mTORC2 critically regulates renal potassium handling. |
News

Immune Response to Malaria and Chagas disease
PD Dr. Thomas Jacobs, Bernhard Nocht Institute for Tropical Medicine, „Immune Response to Infection“ ...
Martinistraße 52
Campus Research N27
20246 Hamburg Germany